BiteSized Immunology: Organs & Tissues

Innate immunity in the large intestine
The intestine is home to about 100 trillion (1×1014) bacteria, both commensal (“friendly”) and pathogenic. To fight infection quickly the intestine has several innate immune defences designed to act immediately when alerted to danger.
Gut morphology and function
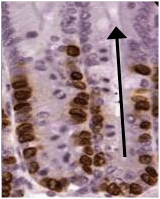
The surface of the intestine is highly folded, forming crypts and villi. Cells move from the base to the tip of the crypt where they are lost into the lumen by anoikis (a kind of apoptosis). The high turnover of epithelial cells can be visualised via the incorporation of BrdU. It takes 5-7 days to travel from the base to the tip (shown by the arrow). This process is accelerated by Th2 cytokines such as IL-13.
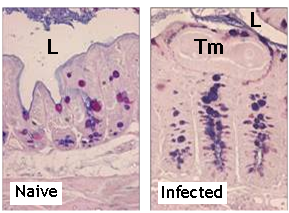
Goblet cells and mucus
Goblet cells are simple columnar epithelial cells which develop from stem cells in the base of the crypt. They contain mucopolysaccharide in secretory granules which expands up to 500-fold after release. LPS from Gram-negative bacteria and Th2 cytokines are goblet cell stimulants. They cause increased expression and exocytosis of MUC5A and 5B.
Mucus protects enterocytes by acting as a physical barrier to the motility and feeding of bacteria and other pathogens such as intestinal parasites. It also contains large quantities of IgA capable of trapping invading bacteria.
Innate effector molecules
Produced by goblet and epithelial cells as well as neutrophils and macrophages in response to numerous pathogens. These molecules are not antigen specific and do not exhibit immunological memory.
Defensins
α- and β-defensins are produced in the intestine and kill a wide spectrum of pathogens in vitro. Low levels of β-defensin-2 are associated with an increased risk of colonic Crohn’s disease.
Cathelicidin
Only one identified in humans; LL37, which is anti-microbial and binds and neutralises LPS.
RELM-b
A goblet cell molecule associated with expulsion of the nematode parasite Trichuris muris.
Innate immune cells
The large intestine is also home to tissue-resident macrophages, eosinophils and mast cells. Between them these cells can phagocytose pathogens and release toxic and inflammatory mediators such as nitrogen radicals and histamine. Neutrophils are often the first cells recruited to a site of inflammation and phagocytose and destroy pathogens using toxic enzymes such as lysozyme and peroxidase.
Pathogen recognition receptors
These include the TLR and NOD families of receptors. Normally expressed on the basal side of the epithelial layer or even intracellularly to avoid activation by the normal flora, they are ideally placed to alert the immune system to the presence of invading pathogens. Detection of pathogen-associated molecular patterns by these receptors initiates a powerful inflammatory response.
© The copyright for this work resides with the author.