BiteSized Immunology: Organs & Tissues

Transplant rejection: T-helper cell paradigm
Transplants that are from a genetically unrelated donor of the same species are termed allografts. Allogeneic transplantation is deemed the last resort for the treatment of chronic organ failure. Even with the aid of organ preservation and the advances in immunosuppression, the major complication post-transplantation is rejection. Rejection occurs despite pre-transplant tissue typing/blood analysis and is seen in almost all transplant recipients, to varying degrees. Outside hyperacute rejection, which occurs due to the presence of pre-existing antibodies (resulting from pregnancy, blood transfusions and/or previous transplants), transplant rejection (Figure 1) can be split broadly into two types; acute and chronic. Acute rejection is thought to be solely an immunological response, whereas chronic rejection involves both immunologic and non-immunologic mechanisms.
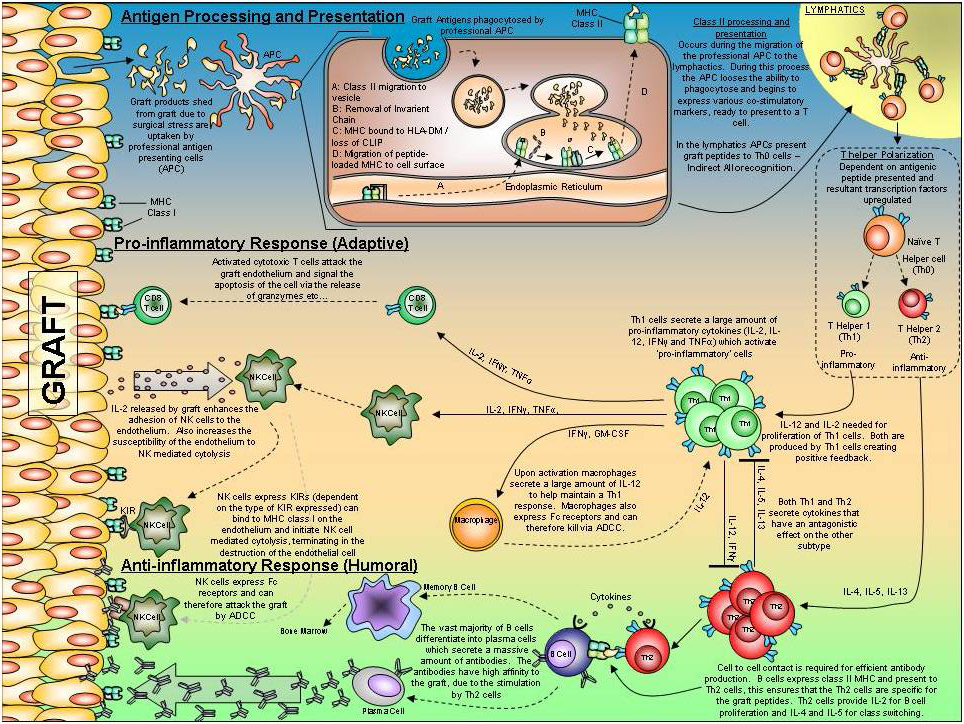
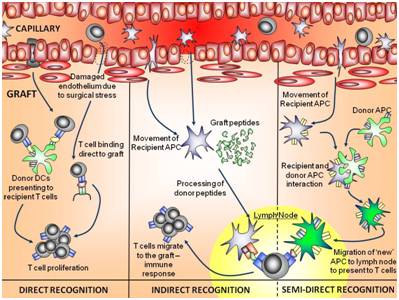
Allorecognition (Figure 2) is the processing and presentation of graft antigen (alloantigen) and is divided into two main subtypes: direct and indirect. Dendritic cells migrating from the graft initiate direct allorecognition, where recipient T cells recognise allogeneic MHC plus associated peptides directly. Later, recipient APCs pick up fragments of donor MHC and present allogeneic peptides to recipient T cells in association with self-HLA (indirect allorecognition). A third subtype, semidirect allorecognition, involving transfer of donor MHC to host cells, has also been proposed. Naïve CD4+ T helper cells (nTh) are one of the first immune cells to be activated post-transplant, playing a key role in rejection. Activated nTh develop into either Th1 (pro-inflammatory) or Th2 (anti-inflammatory) subtypes. Each subtype orchestrates a characteristic, immune response profile (each being mutually suppressive). In the presence of TGF-β and IL-6, nTh differentiate into Th17 cells, a novel subset of Th cells that secrete IL-17 whose role in transplant immunology is still unclear.
A Th1 response is correlated with acute rejection episodes with the production of pro-inflammatory cytokines – IFNγ, IL-2, IL-12, TNFα and GM-CSF. This cytokine profile activates macrophages, natural killer (NK) cells and cytotoxic T cells (Tc) which are drawn to the graft. Tc attack by releasing perforin, which creates pores in the graft endothelium; granzymes released from the Tc then enter the cell, and activate caspases which induce cell apoptosis (cytolytic granule exocytosis pathway).
Activated NK cells have a number of effector functions at their disposal: cytolytic granule exocytosis, death receptor expression (FASL + TRAIL), antibody dependent cell-mediated cytotoxicity (ADCC) and cytokine secretion. Activated macrophages can orchestrate and maintain a localised pro-inflammatory response against the graft via cytokine release (IFNγ and IL-12).
An anti-inflammatory allogenic response predominantly sees a Th2 phenotype, which has a strong correlation with chronic rejection. Th2 cells result in the activation of B cells. Cell-to-cell contact and cytokine exchange between both Th2 and B cell is required for antibody production towards the graft. B cells express MHC class II, which present to Th2 cells (indirect), resulting in Th2 activation/proliferation. The resultant Th2 cells are specific for the alloantigen presented initially by the B cell and secrete IL-2 for B-cell proliferation and IL-4 and -5 for antibody class switching. The bulk of activated B cells differentiate into antibody secreting plasma cells (mainly IgG and IgM) with specificity towards the graft. Attachment of Ab to the graft endothelium eventually leads to the activation of complement, resulting in cell lysis. Alternatively, B cells develop into memory cells and return to the bone marrow, developing an immunological memory towards the graft.
© The copyright for this work resides with the author.