BiteSized Immunology: Immune Development

Neonatal Immunology
Introduction
Like many other systems in the body, the immune system is not fully functional at birth and therefore we are at an increased risk of infection. At the same time, the act of being born – moving from the sterile environment of the womb to the wider world, exposes us to a whole range of pathogens that we have never encountered and have no protection against. To supplement this period of immune immaturity and reduce the risk of infection, the mother transfers passive protection to the child, mainly in the form of antibody.
The immune response in early life is dampened compared to adults. This in part is caused by the immunosuppressive environment of the womb. Speculatively though it may also be an adaption to the exposure to larges amounts of new antigens in early life. The immune response is carefully regulated to ensure appropriate levels of immune response but avoiding inflammatory responses to benign or harmless antigens. Since there are more new antigens in early life, it may be that the response is skewed to suppression.
The reduction in immune response leads to increased susceptibility to pathogens and to reduced responses to vaccines that are effective in adults, necessitating research on infant-specific formulations. The altered function of the neonatal immune response may also influence the development of asthma and allergy in later life.
Importance
Five million infants die in the first year of life, 1.5 million of these deaths are due to infection. The most common causes are respiratory infection and diarrhoea. Sadly, current vaccines are not as effective in early life as they are in adulthood.
Development of the immune system
In many ways the immune system we are born with is the product of the immune environment during pregnancy. In order to maintain the foetus the mother needs to ignore the foetal alloantigens (half of the antigens being of paternal, and therefore of foreign origin). This leads to a scenario of immunosuppression/regulation during pregnancy and this carries over into early life. (For more about cellular development see: T-cell development in the thymus).
Transfer of protection from mother-to-child
The main component of immune protection transferred from mother to child is antibody. This is transferred across the placenta to the foetus using the FcRn (neonatal Fc receptor). Antibody is also transferred to the infant via breast milk. The main immunoglobulin class transferred is IgA, the transferred IgA works at mucosal surfaces, where it is able to prevent pathogen entry. However other important factors are transferred, including complement and commensal bacteria – which may provide protection against asthma and allergy in later life (see: Complement system).
Features of the neonatal immune system
Pattern recognition: Neonatal responses to pathogen associated molecular patterns (PAMPs) are reduced compared to adults. However pattern recognition receptor (PRR)-expression levels are similar. It appears that the molecules that transduce the signal (for example interferon response factor 3 – IRF3) have reduced function. This leads to reduced production of key inflammatory mediators, for example interleukin-12 (IL-12) and interferon-α (IFNα). PRR function increases over time, and the increase in capacity occurs in proportion to time since birth rather than ‘gestational’ age, suggesting that it is controlled by exposure to the environment and removal of maternal influence.
T-cell response: There is a well-documented skewing of the neonatal T-cell response towards T helper 2 (Th2). This is associated with the reduction in IL-12 and IFNα production by neonatal antigen-presenting cells (APC). This may have an effect on the immune response to antigens seen in early life – possibly inducing an allergic type response.
B-cell response: Antibody production in early life is reduced. In particular the antibody response to polysaccharide antigens is reduced. This is a particular problem with regards to bacterial infections, to which newborn children are highly susceptible. This failure to produce antibody is associated with several factors including reduced T cell help, fewer follicular dendritic cells and germinal centres and reduced signalling through the CD40 ligand family members.
Downstream effects of the neonatal immune response
The immaturity of the neonatal immune response has an effect on three important areas:
1. Increased susceptibility to infection. The recognition of infectious agents is reduced in early life and it is therefore easier for a pathogen to invade the host. Neonates are also less experienced so have no immune memory against infection.
2. Decreased vaccine efficacy. In a similar fashion to infection, reduced recognition of vaccine antigens as foreign means that induction of protective memory responses to vaccines are reduced. There is also an effect of maternally derived antibody which may mask key epitopes of the vaccine.
3. Development of asthma and allergy. The Th2 skewing of the T cell response is hypothesised to drive the development of allergic responses to antigen in early life.
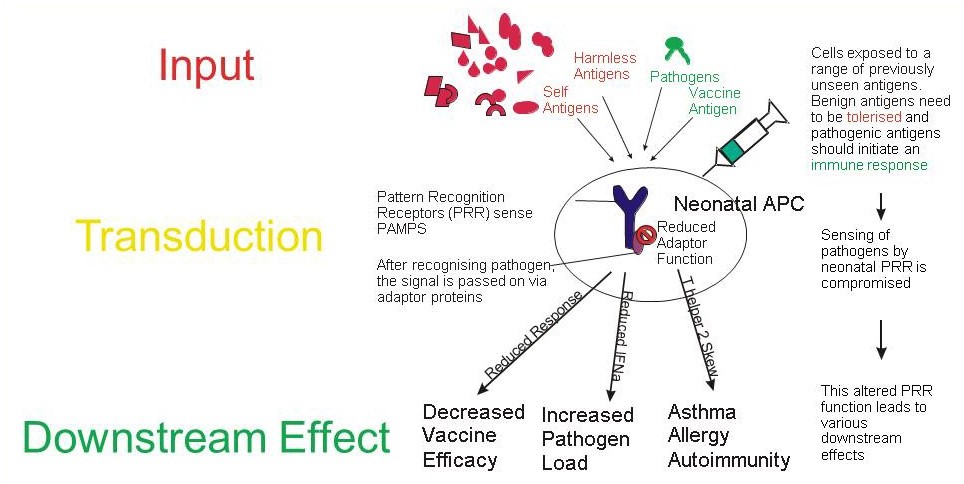
The neonatal immune system is exposed to a large number of previously unseen antigens. The majority of these antigens are benign and therefore should be tolerised but some are dangerous and therefore should induce an immune response. The neonatal antigen presenting cells (APC) have reduced recognition of antigens regardless of source (self, benign, pathogenic, vaccine). This is mediated at the level of pattern recognition receptors (PRR) or their adaptor molecules. This leads to reduced immune responses to these antigens and has an impact on vaccine efficacy, disease susceptibility and, possibly by skewing responses to Th2, the development of asthma and allergy.
© The copyright for this work resides with the author.
This article was updated in 2022