BiteSized Immunology: Pathogens & Disease

Immune responses to fungal pathogens
There are 1.5 - 5 million species of fungi which have the ability to grow almost anywhere including the ocean, soil, plants and animals. Some form spores which we inhale on a daily basis (e.g. Aspergillus species), and others live as human commensal organisms (e.g. Candida species). Despite the close encounters we have with fungi, how our immune system recognises and protects us from fungal pathogens is not as well understood as compared to bacteria or viruses.
Although there are a huge number of fungi in the world, only a small number can cause disease. Most of the disease-causing fungi are opportunistic pathogens, meaning they only cause disease under certain circumstances − such as when the immune system becomes weakened. For example, chemotherapy, immunosuppressive drugs and HIV infection all result in an impaired immune system, meaning that fungi can then more easily infect these vulnerable patients. Our increased usage of these types of drugs together with the rise in HIV infections means that the incidence of fungal infections has become much higher in recent decades.
Fungi can cause lots of different types of infections (Table 1). These can range from common skin and mucosal infections, to a serious life-threatening sepsis and organ failure. In both cases, there are few treatments available, and there are no available vaccines.
|
Fungal Species |
Types of Infection |
| Candida albicans | Vulvovaginal candidiasis (thrush)Oral candidiaisis (mouth infection)Disseminated candidiasis (sepsis) |
| Aspergillus fumingatus | Invasive pulmonary aspergillosis (lung infection) |
| Pneumocystis carinii | Pneumonia (lung infection) |
| Cryptococcus neoformans | Cryptococcosis (lung infections, meningitis) |
Table 1. Common fungal pathogens and some of the infections they cause, usually in immunocompromised patients.
Innate recognition of fungi by the immune system
Fungi are recognised by cells of the innate immune system (e.g. dendritic cells and macrophages) which bind components of fungal cell walls using pattern recognition receptors (PRRs) on their surface. C-type lectin receptors (CLRs, e.g. Dectin-1) are particularly important PRRs in anti-fungal immunity, although several other PRRs are also involved including the Toll-like receptors (TLRs, e.g. TLR2) (Figure 1).
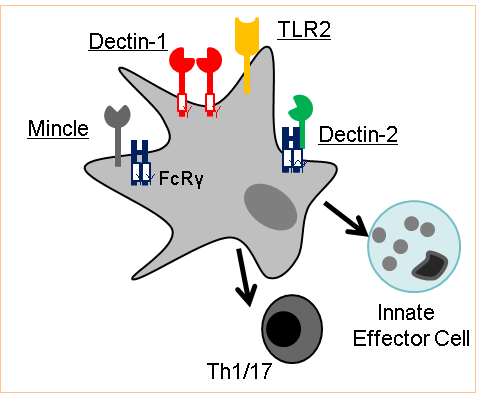
When PRRs bind fungi, they signal using their intracellular tails or associated molecules (FcRγ) resulting in phagocytosis, initiation of killing mechanisms (e.g. production of reactive oxygen species) and also help drive the development of adaptive immunity. Adaptive immunity to fungi is only partially understood, although it seems that CD4+ T-cells that make IFNγ (Th1) or IL-17 (Th17) provide the best protection during fungal infections, as these help drive effective killing by innate effector cells such as neutrophils and macrophages.
Many CLRs use the same signaling molecule, CARD9, to activate these antifungal immune responses. As a result, mice or humans deficient in CARD9 are highly susceptible to fungal infections, because although they have the PRRs to bind fungi, the receptors can’t signal and therefore there is no immunity. CARD9 is the most important molecule for activating antifungal immune responses discovered to date.
© The copyright for this work resides with the BSI